Key Facts
- Leprosy, also known as Hansen’s disease, is a devastating chronic infectious disease caused by Mycobacterium leprae and Mycobacterium lepromatus.
- The disease predominantly affects the skin and peripheral nerves.
- Left untreated, the disease may cause progressive and permanent disabilities.
- The bacteria are transmitted via droplets from the nose and mouth during close, prolonged and frequent contacts with untreated cases.
- Leprosy is curable with Multiple Drug Therapy (MDT).
- In 2023, a total of 182,815 new cases of Leprosy were reported across all six WHO regions. Of these, 21,043 new cases (11.5%) were reported in the African region.
- People affected by leprosy are often subject to discrimination and stigmatization
Scope of the problem
Leprosy Elimination as a public health problem (defined as end-of-year prevalence rate less than 1 per 10 000 population as per World Health Assembly resolution 44.9 and AFR/RC44/R5), had been achieved and was sustained until 2023 at the regional level and in almost all the Member States of the African Region. However, the leprosy burden and pockets of hotspots remain in many countries with more than 20,000 new cases reported every year in our Region.
During 2023, there were 182 815 new cases reported globally with 21 043 (11.5%) new cases from 45 out 47 countries in African Region corresponding to a rate of detection of 17.2 per million population.
The geographical distribution of new Leprosy cases in 2023 in the Africa region is as follows:
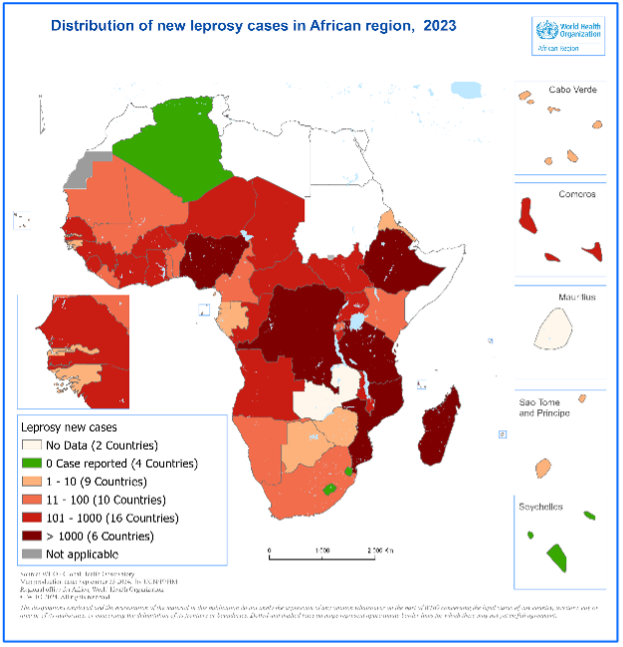
- Four countries reported 0 cases: Algeria, Lesotho, Eswatini, Seychelles.
- Nine countries reported 1 to 10 new cases: Botswana, Cape Verde, Eritrea, Gabon, Gambia, Guinea-Bissau, Equatorial Guinea, São Tomé and Príncipe, Zimbabwe.
- Ten countries reported 11 to 100 new cases: Benin, Cameroon, Kenya, Liberia, Mali, Mauritania, Namibia, Rwanda, Togo, South Africa.
- Sixteen countries reported 101 to 1000 new cases.
- Six countries reported more than 1000 new cases: Democratic Republic of the Congo, Ethiopia, Madagascar, Mozambique, Nigeria, Tanzania.
- 2 countries did not report any cases: Mauritius and Zambia.
The occurrence of new leprosy cases among children serves as a proxy indicator for recent transmission. In 2023, a total of 1,633 new child cases (7.8% of all new cases) were reported in the African Region, corresponding to a rate of 2.6 per million child population. New cases with Grade 2 Disability (G2D) indicate delayed case detection. In the African region, 3,026 new cases with G2D were detected, corresponding to a rate of 2.5 per million population, accounting for 14.4% of all new cases detected during the year. This increase could be linked to the resumption of activities following the COVID-19 pandemic, as well as a decrease in expertise at the country level.
More detailed information on key leprosy indicators is available on The Global Health Observatory.
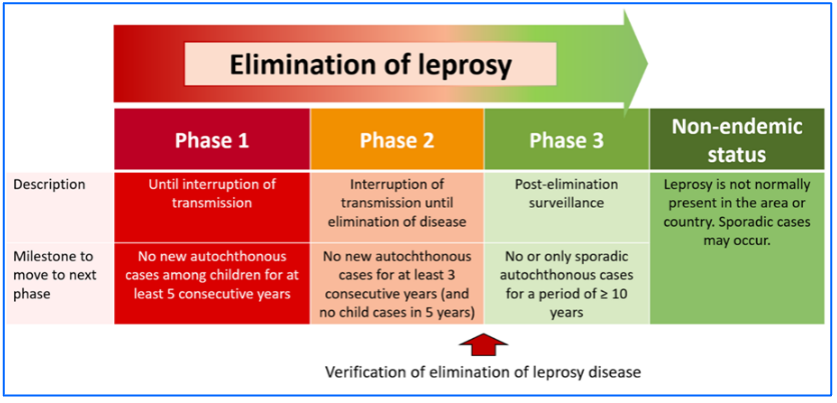
The leprosy situation in the African Region is currently characterized by a slow but steady decline in both detection and prevalence rates. Between 2013 and 2023, the leprosy prevalence rate decreased from 24.4 to 20.4 cases per million, while the detection rate also declined from 22.5 to 17.2 cases per million. Leprosy elimination as a public health problem has been achieved and sustained in almost all countries of the region. Notably, eight out of the 47 countries (17%) in the region have reported no new cases among children for over five years, positioning them close to achieving the interruption of transmission.
Despite these achievements, there remains a need to maintain high-level political commitment and secure continued donor support for essential activities, such as integrated capacity building, active case finding, and the supply and logistics of Multi-Drug Therapy (MDT). These efforts are crucial to achieving the interruption of leprosy transmission by 2030, in line with the new NTDs roadmap targets.
Causative organism
Leprosy is caused by Mycobacterium leprae and Mycobacterium lepromatus, an acid-fast bacterium affecting mainly the skin and nerves.
Transmission
The disease is transmitted through droplets from the nose and mouth. Prolonged, close contact over months with someone with untreated leprosy is needed to catch the disease. The disease is not spread through casual contact with a person who has leprosy like shaking hands or hugging, sharing meals or sitting next to each other. Moreover, the patient stops transmitting the disease when they begin treatment.
Diagnosis
The diagnosis of leprosy is done clinically. Laboratory-based services may be required in cases that are difficult to diagnose or to monitor drug resistance.
 The disease manifests commonly through skin lesion and peripheral nerve involvement. Leprosy is diagnosed by finding at least one of the following cardinal signs: (1) definite loss of sensation in a pale (hypopigmented) or reddish skin patch; (2) thickened or enlarged peripheral nerve, with loss of sensation and/or weakness of the muscles supplied by that nerve; (3) microscopic detection of bacilli in a slit-skin smear.
The disease manifests commonly through skin lesion and peripheral nerve involvement. Leprosy is diagnosed by finding at least one of the following cardinal signs: (1) definite loss of sensation in a pale (hypopigmented) or reddish skin patch; (2) thickened or enlarged peripheral nerve, with loss of sensation and/or weakness of the muscles supplied by that nerve; (3) microscopic detection of bacilli in a slit-skin smear.
Based on the above, the cases are classified into two types for treatment purposes: Paucibacillary (PB) case and Multibacillary (MB) case.
PB case: a case of leprosy with 1 to 5 skin lesions, without demonstrated presence of bacilli in a skin smear.
MB case: a case of leprosy with more than five skin lesions; or with nerve involvement (pure neuritis, or any number of skin lesions and neuritis); or with the demonstrated presence of bacilli in a slit-skin smear, irrespective of the number of skin lesions.
 Leprosy is a curable disease. Early diagnosis and complete treatment with Multiple Drug Therapy (MDT) remain the key strategies for reducing the disease burden of leprosy and help to prevent disabilities.
Leprosy is a curable disease. Early diagnosis and complete treatment with Multiple Drug Therapy (MDT) remain the key strategies for reducing the disease burden of leprosy and help to prevent disabilities.
The 2018 Guidelines for the diagnosis, treatment and prevention of leprosy published by WHO, recommends the same 3-drug regimen with rifampicin, dapsone and clofazimine for all leprosy patients, with a duration of treatment of 6 months for PB leprosy and of 12 months for MB leprosy.
The treatment also includes presentation of disabilities as well as management of reactions and complications.
Early case detection and prompt treatment with MDT, despite having the capacity to reduce leprosy burden, have proven insufficient to interrupt transmission, excepted in very low endemic countries.
The technical guidance for contact tracing and post-exposure prophylaxis published by WHO recommends tracing household contacts along with neighbourhood and social contacts of each patient, accompanied by the administration of a single dose of rifampicin as preventive chemotherapy. This strategy has been implemented in some countries of the African Region such as Benin, Comoros, Nigeria, and Tanzania, and would show impact after a five-year period.
 After detailed consultations with countries, experts, partners and persons affected by leprosy, WHO released the Towards zero leprosy: global leprosy (Hansen’s disease) strategy 2021–2030 aligned to the neglected tropical diseases road map 2021–2030. The Strategy calls for a vision of zero leprosy: zero infection and disease, zero disability, zero stigma and discrimination and the elimination of leprosy (defined as interruption of transmission) as its goal. The four strategic pillars of the strategy include:
After detailed consultations with countries, experts, partners and persons affected by leprosy, WHO released the Towards zero leprosy: global leprosy (Hansen’s disease) strategy 2021–2030 aligned to the neglected tropical diseases road map 2021–2030. The Strategy calls for a vision of zero leprosy: zero infection and disease, zero disability, zero stigma and discrimination and the elimination of leprosy (defined as interruption of transmission) as its goal. The four strategic pillars of the strategy include:
- implementing integrated, country-owned zero leprosy roadmaps in all endemic countries
- scaling up leprosy prevention alongside integrated active case detection
- managing leprosy and its complications and prevent new disability
- and combatting stigma and ensuring human rights are respected.
The Strategy also recognizes that global and national investment in research is essential to achieving zero leprosy and includes a set of key research priorities.
 Research
Research priorities include:
priorities include:
- More effective approaches to active case detection in different contexts and levels of endemicity
- Innovative approaches to building capacity of health workers
- Tools for geospatial distribution of leprosy and surveillance mapping
- Improved preventive approaches including chemotherapy regimen and vaccines
- Tools for epidemiological and programme monitoring
- Diagnostic tests, including at community and point-of-care level, for disease and infection
- Impact of case finding and contact tracing strategies on the number of new cases with disabilities
- Optimized and new treatment options for reactions and nerve function impairment
- Diagnostic tools for detection and monitoring of nerve function impairment and reactions
- Improved understanding of the mechanism of leprosy reactions
- More effective drugs or drug combinations, or shorter regimens, to treat or prevent leprosy
- Improved understanding of transmission including host, agent and environmental factors and zoonotic transmission
- Effective models of care throughout the patient journey
- Digital health applications in leprosy
- Inclusive approaches in community-based rehabilitation and stigma reduction
- New technologies for wound care, orthosis, prosthesis and materials for footwear.
Resolutions and decisions
- Elimination de la lèpre dans la Région africaine | AFR/RC44/R5
- Elimination of leprosy as a public health problem, 1998 | WHA51.15
- Leprosy, 1991 | WHA44.9
- Towards the elimination of leprosy, 1987 | WHA40.35
- Leprosy, 1979 | WHA32.39
- Leprosy control, 1977 | WHA30.36
- Leprosy control, 1976 | WHA29.70
- Leprosy control, 1975 | WHA28.56
- Coordination and strengthening of leprosy control, 1974 | WHA27.58
- Inter-regional Conference on Leprosy Control, 1958 | WHA9.45
- Expert Committee on Leprosy: First Report, 1953 | WHA6.19
- Leprosy, 1952 | WHA5.28
- Studies of Communicable Diseases (Leprosy), 1950 | WHA3.71.3.2
- Leprosy, 1949 | WHA2.43
Databases and tools
- Interactive graph (Global Health Observatory)
- Data repository (Global Health Observatory)
- Annual Request for the supply of free anti-leprosy medicines
Training
Technical work
Publications
- Weekly Epidemiological Record
- Framework for the integrated control, elimination and eradication of tropical and vector-borne diseases in the African Region 2022–2030: report of the Secretariat
- Ending disease in Africa: responding to communicable and noncommunicable diseases, progress report 2020-2022
- Ending disease in Africa: vision strategies and special initiatives, 2023-2030.
- Report of a WHO meeting on skin-related neglected tropical diseases in West Africa, Geneva, 3-5 October 2022
- Ending the neglect to attain the sustainable development goals: a road map for neglected tropical diseases 2021–2030.
- Ending the neglect to attain the sustainable development goals: a strategic framework for integrated control and management of skin-related neglected tropical diseases
- Other publications





 Multiple Drug Therapy (MDT), a combination of three medicines (dapsone, clofazimine and rifampicin) has been the cornerstone of leprosy treatment since the 1980s.
Multiple Drug Therapy (MDT), a combination of three medicines (dapsone, clofazimine and rifampicin) has been the cornerstone of leprosy treatment since the 1980s.
 Skin diseases are the third most prevalent cause of illness and one of the top 10 causes of disability. They are also among the 10 most common causes of outpatient visits.
Skin diseases are the third most prevalent cause of illness and one of the top 10 causes of disability. They are also among the 10 most common causes of outpatient visits.
 WHO has developed
WHO has developed