Key fact

760 000 people
newly infected with HIV in 2022.
Featured video
There are 25.6 million people living with HIV in the African region.
- East and Southern Africa – 20.8 million
- West and Central Africa – 4.8 million
In 2022, about 380,000 people died from AIDS related illness in 2022.
760,000 newly infected with HIV in 2022
- HIV infection is often diagnosed through rapid diagnostic tests (RDTs), which detect the presence or absence of HIV antibodies. Most often these tests provide same-day test results, which are essential for same-day diagnosis and early treatment and care.
- Key populations and their sexual partners accounted for over half of all new infections (an estimated 54%) for the first time in 2018.
- Key populations include: men who have sex with men, people who inject drugs, people in prisons and other closed settings, sex workers and their clients, and transgender people. They are at increased risk of HIV infection irrespective of epidemic type or local context.
- Key populations, their clients and sexual partners accounted for 64% of new HIV infections in West and Central Africa, and for 25% of new HIV infections in the East and Southern African subregion. Key populations and their partners accounted for around 95% of new HIV infections in eastern Europe and central Asia and in the Middle East and North Africa in 2018.
- Key populations often face legal and social barriers that increase their vulnerability to HIV and impede their access to prevention, testing and treatment programmes.
- There is no cure for HIV infection. However, effective antiretroviral (ARV) drugs can control the virus and help prevent transmission so that people with HIV and those at substantial risk, can enjoy healthy, long and productive lives.
- It is estimated that currently 79% of people with HIV know their status. In 2018, an estimated 23.3 million people living with HIV were receiving antiretroviral therapy (ART) globally.
- Between 2000 and 2018, new HIV infections fell by 37%, and HIV-related deaths fell by 45% with 13.6 million lives saved due to ART in the same period. This achievement was the result of great efforts by national HIV programmes supported by civil society and a range of development partners.
No effective cure for HIV exists at present but HIV can be suppressed by a combination of medicines called antiretroviral (ARV) therapy consisting of three or more ARV drugs. Antiretroviral therapy does not cure HIV infection but suppresses viral replication within a person's body and allows an individual's immune system to strengthen and regain the capacity to fight off infections.
People with HIV can enjoy long, healthy lives by taking ARV treatment.
In 2021, WHO released the Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: Recommendations for a public health approach. These consolidated guidelines on preventing and treating HIV infection bring together a series of recommendations to promote the highest quality, person- centered delivery of care for people living with HIV and affected by HIV
HIV still causes too many avoidable deaths, but by providing the right health services in a timely manner, we can avoid the worst consequences of the virus. The recommendations in these guidelines aim to reduce the number of people dying from HIV and, when fully implemented, will help us to reach our goals of reducing global HIV deaths to less than 200 000 by 2030. For most people living with HIV, it is a chronic, lifelong condition. Evidence and lived experience have shown that with the right support, people are able to manage their own health according to what works best in their lives. The service delivery approaches put forward in these guidelines aim to promote self-management for the majority of people living with or affected by HIV. This includes an expanded range of options for diagnosing, preventing, and treating HIV that are delivered and monitored in the community.
Treatment and care in children and adolescents
In the African region, an estimated 1.3 million children aged 0-14 were living with HIV at the end of 2022, and 109 000 children were newly infected. An estimated 69 000 children died of AIDS-related illnesses. To reduce HIV-related mortality and morbidity among this highly vulnerable population, early testing and treatment is essential. Without access to testing and treatment, 50% of children with HIV will die by the age of 2, and 80% will not live to their fifth birthday.
WHO recommends that infants born to mothers living with HIV are tested for HIV, at birth, six weeks, during breastfeeding, and when breastfeeding ends given the continued risk of transmission during this period. Older children, especially offspring and siblings of persons infected with HIV, should also be tested.
HIV-positive children should be started on antiretroviral drugs (ARV) immediately. Once treatment begins, children must take their medicine regularly to stay healthy into adolescence and adulthood. Failure to suppress the HIV virus remains a serious problem among children, aggravated by a lack of child-friendly formulations of the newest and most effective ARVs designed for adults.
Compared to other populations, adolescents face additional barriers in accessing testing and treatment, including health services that are not adapted to their needs and policies that require parental consent for services. HIV-positive adolescents also are less likely than adults to adhere to their treatment regularly, resulting in lower rates of viral suppression and lower declines in mortality.
Addressing the distinct and diverse needs of adolescents living with HIV to improve their HIV-related outcomes requires a comprehensive and integrated approach that leverages on global commitments and approaches to adolescent health, including the Global Strategy for Women, Children, and Adolescents’ Health (2016–2030) and the Global Accelerated Action for the Health of Adolescents (AA-HA!).
WHO recommends the implementation of adolescent-friendly health services in HIV services to ensure engagement and improved outcomes. Involving and engaging in their own care across the treatment cascade and through the cycle of planning, implementing, monitoring and evaluating programs is key. Peer-driven, adolescent-friendly services, integrated with other services including psychosocial interventions, are effective ways to improve health outcomes for adolescents.
HIV Drug Resistance
Tens of millions of HIV/AIDS patients have had their lives saved thanks to the extraordinary rise in the use of antiretroviral medication (ART) during the last ten years. Of the estimated 25.6 million people living with HIV in the African region, 20.8 million were on antiretroviral therapy (ART) as of the end of 2022.
HIV drug resistance has emerged in tandem with the growing usage of HIV medications; in recent years, the prevalence of this resistance has been progressively rising. Changes in the genetic makeup of HIV impact the medications' capacity to prevent the virus from replicating, leading to HIV drug resistance. Due to the advent of newer kinds of antiretrovirals, all currently available medications have the potential to become partially or completely inactive.
Drug-resistant virus strains have the potential to render all antiretroviral medications, including those from more recent classes, partially or completely inert. HIV drug resistance has the potential to compromise antiretroviral medication effectiveness if it is not addressed, leading to a rise in HIV infections as well as higher rates of morbidity and mortality related to HIV.
- Guidelines on the public health response to pretreatment HIV drug resistance
- WHO releases HIV drug resistance report 2021
• WHO urges action against HIV drug resistance threat
Prevention of HIV drug resistance
WHO recommends assessing whether antiretroviral therapy (ART) programmes are delivering services at the quality required, to minimize the emergence of HIV drug resistance. This assessment is achieved with a set of standard quality-of-care indicators known as “early warning indicators” of HIV drug resistance.
The early warning indicators use standardized definitions, which have evolved over time as programmes mature and public health actions are refined. The most up-to-date set of early warning indicators for HIV drug resistance are included in the WHO “Consolidated HIV Strategic Information Guidelines” and the HIV Drug Resistance Strategy, 2021 update.
- Total attrition from ART
- People living with HIV who have suppressed viral load
- Viral load testing coverage
- Timely second viral load test
- ARV medicine stock-out
- ART adherence proxy (ARV refills)
- Timely switch to second-line ART
- Consolidated guidelines on person-centred HIV strategic information: strengthening routine data for impact
- HIV drug resistance strategy, 2021 update
Policy brief
- Policy brief on integrating and strengthening monitoring of differentiated ART service delivery
- Policy brief on digital health data
- Enhancing the monitoring of HIV testing and treatment
Laboratory network for HIVDR
The WHO HIV drug resistance laboratory network supports HIV drug resistance surveys by providing accurate and timely genotyping results that meet WHO specifications.
Its objectives are to ensure:
- the proper collection, handling, shipment and storage of specimens; and
- the availability of quality-assured HIV genotyping laboratory services producing comparable and reliable results at the national, regional and global level.
The national HIV drug resistance working groups that coordinate WHO-recommended surveys must use a WHO-designated genotyping laboratory to provide quality-assured testing services for drug resistance surveys.
To be designated as a laboratory for WHO surveys, several mandatory criteria must be met including a site inspection and annual external proficiency testing. The roles and responsibilities of network laboratories, recommended testing, internal and external quality assurance procedures, and assay validation recommendations are summarized in the WHO/HIVResNet HIV drug resistance laboratory operational framework.
- Minimum criteria for external quality assurance proficiency tests for use by laboratories designated by WHO for HIV drug resistance surveillance
- Target product profile for HIV drug resistance tests in low- and middle-income countries: Africa
- WHO manual for HIV drug resistance testing using dried blood spot specimens
- WHO HIVResNet HIV drug resistance laboratory operational framework
HIV drug resistance surveillance
Global and national policy decisions on antiretroviral therapy and HIV service delivery need to be informed by reliable national data on HIV drug resistance (HIVDR) prevalence and trends. HIV treatment and pre-exposure prophylaxis scale-up should be accompanied by measures to monitor the quality of antiretroviral drug delivery and surveillance of HIVDR.
Quality data should be obtained from periodic nationally representative HIVDR surveys among different populations.
- Laboratory-based survey of acquired HIV drug resistance using remnant viral load specimens
- Clinical-based survey of acquired HIV drug resistance
- Sentinel surveys of acquired HIV resistance to dolutegravir among people receiving dolutegravir-containing antiretroviral therapy
Surveillance of pretreatment HIV drug resistance- populations initiating first-line ART
Pretreatment HIV drug resistance is detected among people initiating antiretroviral therapy (ART) with or without prior antiretroviral drug exposure. It can result from transmitted or acquired HIV drug resistance, or both. Surveillance of the pre-treatment HIV drug resistance survey in populations initiating first-line ART is relevant to inform the choice of nationally recommended first-line ART regimens, and also regimens used for pre- and post-exposure prophylaxis.
Surveillance of pretreatment HIV drug resistance- treatment -naïve infants newly diagnosed with HIV
The surveillance of pretreatment HIV drug resistance among treatment-naive infants newly diagnosed with HIV is particularly relevant in settings where many infants acquire HIV infection. Surveillance provides critical information to support optimal choice of first- and second-line antiretroviral therapy regimens.
The purpose of this surveillance is to assess the prevalence of HIV drug resistance among treatment-naive infants younger than 18 months (regardless of prevention of mother-to-child transmission exposure), who have been newly diagnosed with HIV using early infant diagnosis over a 12-month period.
Surveillance of HIV drug resistance- PrEP users diagnosed with HIV
WHO recommends pre-exposure prophylaxis (PrEP) as an additional prevention option for HIV-negative individuals at substantial risk of HIV infection, as part of combination prevention approaches. HIV drug resistance was rarely reported among PrEP users diagnosed with HIV in randomized controlled trials or open-label studies.
However, PrEP-selected HIV drug resistance could potentially negatively impact the effectiveness of antiretroviral therapy (ART) options among PrEP users who acquire HIV. This is because there is a potential for overlapping resistance profiles between antiretroviral drugs used for both PrEP and first-line ART.
Therefore, WHO recommends that PrEP scale-up be accompanied by surveillance of HIV drug resistance, as resistance may compromise the effectiveness of first-line ART among PrEP users who acquire HIV.
The symptoms of HIV vary depending on the stage of infection. Though people living with HIV tend to be most infectious in the first few months, many are unaware of their status until later stages. In the first few weeks after initial infection, individuals may experience no symptoms or an influenza-like illness including fever, headache, rash, or sore throat.
As the infection progressively weakens the immune system, an individual can develop other signs and symptoms, such as swollen lymph nodes, weight loss, fever, diarrhoea and cough. Without treatment, they could also develop severe illnesses such as tuberculosis, cryptococcal meningitis, severe bacterial infections and cancers such as lymphomas and Kaposi's sarcoma, among others.
Tuberculosis (TB) remains the leading cause of death among people living with HIV, accounting for around one in three AIDS-related deaths.
HIV can be transmitted via the exchange of a variety of body fluids from infected individuals, such as blood, breast milk, semen and vaginal secretions. Individuals cannot become infected through ordinary day-to-day contact such as kissing, hugging, shaking hands, or sharing personal objects, food or water.
Risk factors
There is a greater risk of contracting HIV through:
- having unprotected anal or vaginal sex;
- having another sexually transmitted infection such as syphilis, herpes, chlamydia, gonorrhoea, and bacterial vaginosis;
- sharing contaminated needles, syringes and other injecting equipment and drug solutions when injecting drugs;
- receiving unsafe injections, blood transfusions, tissue transplantation, medical procedures that involve unsterile cutting or piercing; and/or
- sustaining accidental needle stick injuries, including among health workers.
HIV infection can be detected with great accuracy, using WHO prequalified tests within a validated approach. No single HIV test can provide an HIV-positive diagnosis. It is important that these tests be used in combination and in a specific order that has been validated and is based on HIV prevalence of the population being tested.
Serological tests, such as rapid diagnostic tests (RDTs) or enzyme immunoassays (EIAs), detect antibodies produced by an individual as part of their immune system to fight off foreign pathogens, rather than direct detection of HIV itself.
Most individuals develop antibodies to HIV within 28 days of infection and therefore antibodies may not be detectable early, during the so-called “window period”. This early period of infection represents the time of greatest infectivity; however, HIV transmission can occur during all stages of the infection.
It is best practice to also retest all people initially diagnosed as HIV-positive before they enrol in care and/or treatment to rule out any potential testing or reporting error. Notably, once a person diagnosed with HIV has started treatment, they should not be retested.
Testing and diagnosis of HIV-exposed infants has been a challenge because babies carry their biological mothers’ antibodies and it can take months for these to disappear. For infants and children less than 18 months of age, serological testing is not sufficient to identify HIV infection: virologic testing must be provided (at 6 weeks of age, or at birth) to detect the presence of the virus in infants born to mothers living with HIV.
HIV infection can be detected with great accuracy, using WHO-prequalified tests with a validated approach. No single HIV test can provide an HIV-positive diagnosis. It is important that these tests be used in combination and in a specific order as in the approved national algorithm.
HIV testing should be voluntary – a person has the right to refuse to be tested. Mandatory or coerced testing by a health care provider, authority, or by a partner or family member is not acceptable as it undermines good public health practice and infringes on human rights.
Serological tests, such as rapid diagnostic tests (RDTs) or enzyme immunoassays (EIAs), detect antibodies produced by an individual as part of their immune system to fight off foreign pathogens, rather than direct detection of HIV itself.
Most individuals develop antibodies to HIV within 28 days of infection and therefore antibodies may not be detectable early, during the so-called “window period”. This early period of infection represents the time of greatest infectivity; however, HIV transmission can occur during all stages of the infection.
Testing and diagnosis of HIV-exposed infants- has been a challenge because babies carry their biological mothers’ antibodies and it can take months for these to disappear. For infants and children less than 18 months of age, serological testing is not sufficient to identify HIV infection: virologic testing must be provided (at 6 weeks of age, or at birth) to detect the presence of the virus in infants born to mothers living with HIV.
HIV self-testing – is an approach where a person collects his or her own specimen (oral fluid or blood) and then performs an HIV test and interprets the result, often in a private setting, either alone or with someone he or she trusts.
- Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: Recommendations for a public health approach
- Laboratory and point-of-care diagnostic testing for sexually transmitted infections, including HIV
Policy briefs
- WHO encourages countries to adapt HIV testing strategies in response to changing epidemic
- WHO recommends HIV self-testing evidence update and considerations for success
- Consolidated guidelines on HIV testing services for a changing epidemic
- What works for generating demand for HIV testing services
- Dual HIV/Syphilis rapid diagnostic tests can be used as the first test in antenatal care
- WHO recommends social network-based HIV testing approaches for key populations as part of partner services package
- WHO recommends countries move away from the western blotting and line immunoassays in HIV testing strategies and algorithms
Toolkit
WHO recommends a combination prevention approach, tailored to the population and reflecting the epidemiology of the setting.
Combination prevention programmes are rights-based, evidence-informed, and community-owned programmes that use a mix of biomedical, behavioural, and structural interventions, prioritized to meet the HIV prevention needs of individuals and communities, to have the greatest sustained impact on reducing new infections.
WHO supports the appropriate integration of hepatitis and sexually transmitted infection prevention, testing and treatment and the inclusion of services which address sexual and reproductive health and mental health issues, which are also critical to acceptable and effective programming.
For HIV and STIs
Testing for HIV and other STIs is strongly advised for all people exposed to any of the risk factors. Through testing, people learn of their own infection status and access necessary prevention and treatment services without delay. WHO also recommends offering testing for partners or couples. Additionally, WHO is recommending assisted partner notification approaches so that people with HIV receive support to inform their partners either on their own, or with the help of health care providers.
Linkages to tuberculosis care
Tuberculosis (TB) is the most common presenting illness and cause of death among people with HIV. It is fatal if undetected or untreated and is the leading cause of death among people with HIV, responsible for more than one out of three HIV-associated deaths.
Early detection of TB and prompt linkage to TB treatment and ART can prevent these deaths. TB screening should be offered routinely at HIV care services and routine HIV testing should be offered to all patients with presumptive and diagnosed TB. Individuals who are diagnosed with HIV and active TB should urgently start effective TB treatment (including for multidrug-resistant TB) and ART. TB preventive therapy should be offered to all people with HIV who do not have active TB.
Voluntary medical male circumcision for HIV prevention
Reaching the 2030 HIV incidence goals in high-burden settings, particularly in Eastern and Southern Africa, and then keeping HIV incidence at low levels, will require the right combination of effective prevention interventions at high coverage levels.
In 2007, the Joint United Nations Programme on HIV/AIDS and WHO recommended voluntary medical male circumcision (VMMC) to reduce the risk of men acquiring HIV infection during heterosexual exposure. The recommendation was based on strong evidence from randomized controlled trials showing an approximately 60% lower risk.
Since 2007, more than 27 million VMMC procedures have been performed in the 15 priority countries in Eastern and Southern Africa, where about half of all new HIV infections occurred. In the past 10 years, other evidence-based HIV prevention options have also been scaled up, including oral pre-exposure prophylaxis and HIV antiretroviral therapy (with its secondary HIV prevention effect), along with already known interventions, such as condom use and post-exposure prophylaxis.
In the ongoing effort to end the AIDS epidemic, a re-examination of the evidence shows that VMMC remains an important intervention, alongside other effective behavioural and biomedical HIV prevention interventions. VMMC should be supported as a key HIV prevention option, within combination prevention for adolescents 15 years and older and adult men in settings with generalized HIV epidemics.
- Preventing HIV through safe voluntary medical male circumcision for adolescent boys and men in generalized HIV epidemics: recommendations and key considerations.
- Assessing and enhancing sustainable voluntary medical male circumcision services for HIV prevention in East and Southern Africa: a landscape report of voluntary medical male circumcision priority countries
Prevention benefits of ART
The WHO recommendation to initiate ART for all people living with HIV will contribute significantly to reducing HIV transmission.
Pre-exposure prophylaxis (PrEP)
Pre-exposure prophylaxis or “PrEP” is the use of an antiretroviral medication by HIV-negative people to reduce the risk of HIV acquisition.
As of September 2015, WHO recommends that people at substantial risk of HIV infection should be offered tenofovir disoproxil fumarate (TDF)-based oral PrEP as an additional prevention choice, as part of comprehensive prevention. Oral PrEP is highly effective at preventing HIV when used as directed. In 2021, WHO recommended that the dapivirine ring may be offered as an additional prevention choice for women at substantial risk of HIV and, in 2022, that long-acting injectable cabotegravir (CAB-LA) may be offered as an additional prevention choice for people at substantial risk of HIV. Other products (e.g., multipurpose prevention products that combine antiretroviral drugs with contraception) are currently studied as additional PrEP options.
- Implementation tool for pre-exposure prophylaxis of HIV infection – integrating STI services
- Guidelines on long-acting injectable cabotegravir for HIV prevention
- Differentiated and simplified pre-exposure prophylaxis for HIV prevention
- Prevention and control of sexually transmitted infections (STIs) in the era of oral pre-exposure prophylaxis (PrEP) for HIV
- What’s the 2+1+1? Event-driven oral pre-exposure prophylaxis to prevent HIV for men who have sex with men: Update to WHO’s recommendation on oral PrEP
- Preventing HIV during pregnancy and breastfeeding in the context od PrEP
Post-exposure prophylaxis for HIV (PEP)
Post-exposure prophylaxis (PEP) is the use of ARV drugs within 72 hours of exposure to HIV to prevent infection. PEP includes counselling, first-aid care, HIV testing, and administration of a 28-day course of ARV drugs with follow-up care. WHO recommends PEP use for both occupational and non-occupational exposures and for adults and children.
People who inject drugs can take precautions against becoming infected with HIV by using sterile injecting equipment, including needles and syringes, for each injection and not sharing drug-using equipment and drug solutions. Treatment of dependence, and in particular opioid substitution therapy for people dependent on opioids, also helps reduce the risk of HIV transmission and supports adherence to HIV treatment. A comprehensive package of interventions for HIV prevention and treatment includes:
- needle and syringe programmes;
- opioid substitution therapy for people dependent on opioids and other evidence-based drug dependence treatment;
- HIV testing and counselling;
- HIV treatment and care;
- risk-reduction information and education and provision of naloxone;
- access to condoms; and
- management of STIs, tuberculosis and viral hepatitis.
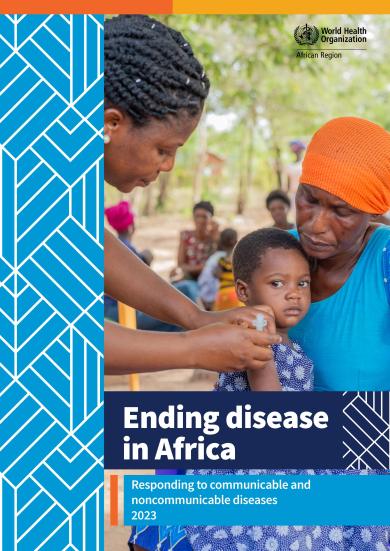
In the African region, a number of women and girls living with HIV become pregnant each year. In the absence of intervention, the rate of transmission of HIV from a mother living with HIV to her child during pregnancy, labour, delivery or breastfeeding ranges from 15% to 45%. As such, identification of HIV infection should be immediately followed by an offer of linkage to lifelong treatment and care, including support to remain in care and virally suppressed and an offer of partner services.
Elimination of MTCT of HIV is strongly supported by global commitments and the promotion of integration of prevention of MTCT interventions into maternal, newborn, child and adolescent health services, as well as strengthened health systems. In addition, improved access to sexual and reproductive health services – including preventing unintended pregnancies and screening and treatment for sexually transmitted infections in women and girls living with HIV – is being actively promoted.
The integration of interventions has led to the triple elimination initiative, which not only promotes person-centered care, but also reduces incidence, morbidity and mortality. The initiative also strengthens disease monitoring using strategic information for response planning.
Essential triple EMTCT services include:
- Testing for HIV, syphilis and HBV in antenatal care clinics.
- Prompt and efficacious interventions to treat women who test positive, and to prevent transmission of the infection(s) to their children.
- Counselling for women and their partners to reduce transmission risk and ensure appropriate treatment.
- Appropriately attended, safe delivery.
- Appropriate follow-up of exposed infants, including HBV vaccine birth dose.
- Optimal infant feeding; and
- Lifelong treatment and care for mothers living with HIV, or eligible for treatment for HBV or syphilis.
WHO continues to work in this area, supporting countries to improve and better monitor interventions towards ending the AIDS epidemic as a public health threat by 2030.
Validation of elimination of mother-to -child transmission of HIV, syphilis and hepatitis B
The global and regional community has committed itself to the elimination of mother-to-child transmission (EMTCT) of HIV, syphilis, and hepatitis B virus (HBV) as a public health priority. The Triple EMTCT initiative focuses on a harmonized approach to improving health outcomes for mothers and children.
The term validation is used to attest that a country has successfully met the criteria for EMTCT of HIV, syphilis, and HBV. WHO develops and regularly updates guidance on the criteria and processes for validation of EMTCT of HIV, syphilis and HBV. Since 2015, Member States have been able to apply for validation for achieving the reduction of mother-to-child transmission (MTCT) to a level where it is no longer a public health threat or problem. In 2017, the Path to Elimination was introduced to recognize countries with high prevalence of maternal HIV, syphilis or HBV in their efforts to reduce MTCT.
Achieving validation of EMTCT is a tremendous national accomplishment, requiring country-led accountability, rigorous data analysis, intensive programme assessment and multilevel collaboration. Maintaining validation is equally important and requires sustained, broad programme efforts to prevent new infections in infants, children and adults. Through the validation process, WHO and partners continue to provide country support for strengthening health system capacity and comprehensive person-centered, integrated services that respect and protect the human rights of women living with any of the conditions, and to ensure that these women are meaningfully involved in health programme planning and service delivery.
- Global guidance on criteria and processes for validation: elimination of mother -to-child transmission of HIV, syphilis and hepatitis B.
- Governance for the validation of elimination of mother to child transmission of HIV, syphilis and hepatitis B virus: an overview of validation structures and responsibilities at national, regional and global levels