Mubende, Uganda – As soon as the Sudan ebolavirus was detected in Uganda and an outbreak was declared on 20 September 2020, the country’s health authorities placed emphasis on supportive care, as no effective vaccine for this species of ebolavirus has yet been licenced.
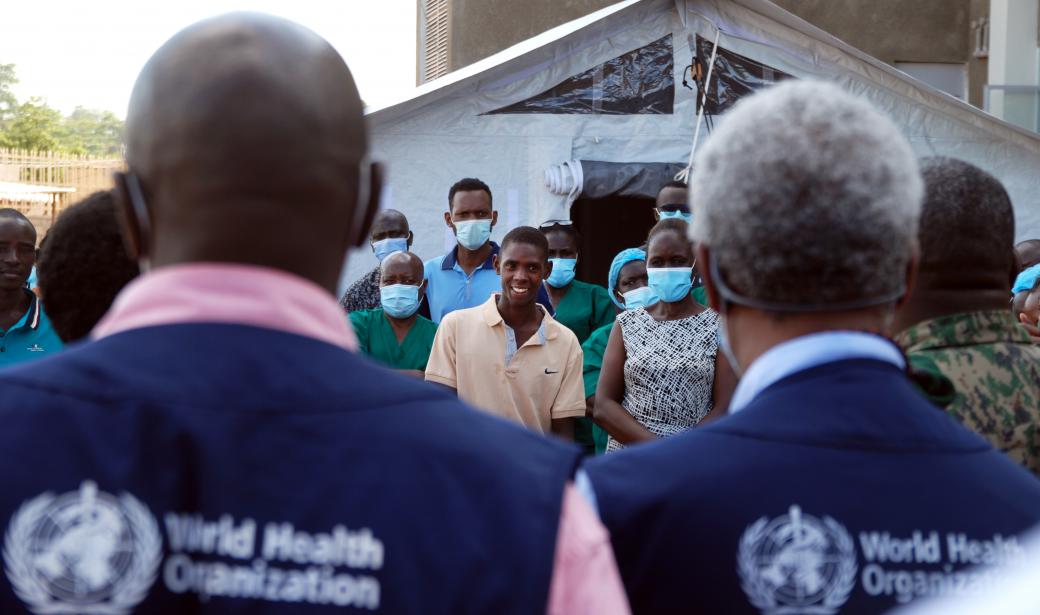
With support from the World Health Organization (WHO) and other partners, they promptly set up an Ebola treatment centre at the Mubende Regional Referral Hospital, where the first case had been detected, and deployed health workers and emergency services to the site.
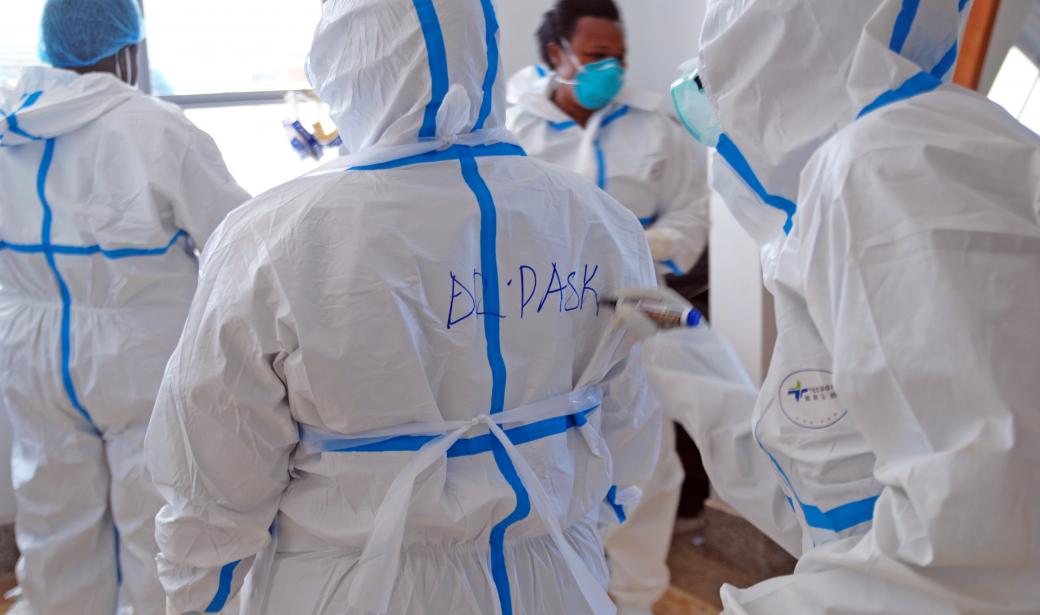
In addition to training doctors, clinical officers and nurses in case management and infection prevention and control, WHO has also provided sufficient Ebola kits to treat 100 patients as it seeks to help Uganda overcome the outbreak as swiftly as possible.
A sample was taken from one such patient and sent to the Uganda Virus Research Institute. “In the evening, we had confirmation that this patient was positive for Ebola,” Adam says. The next day, an Ebola outbreak was officially declared by the government.
“As soon as Ebola was confirmed, we set up a small isolation unit where we transferred all suspected patients,” she recounts. “We were a team of five health workers. We didn’t shy away from the situation. As a nurse, I’m very proud because we worked 24/7 and we remained calm.”
About 10 days after the outbreak was declared, Adam still spends long days working at the back of the hospital compound, where the rapid response team continues to bolster the outbreak response. “We are already seeing improvement in patient care… they are doing better,” she says.
At the start of the outbreak, WHO quickly provided the regional referral hospital with three Ebola treatment kits. Each kit contains enough medical supplies to treat 100 patients.
With support from Médecins Sans Frontières (MSF) and other United Nations aid agencies, an isolation tent with 12 beds for confirmed cases was set up at the centre just five days after the outbreak was declared. Shortly after, it was complemented with another tent equipped with 24 beds and all the necessary medical equipment to monitor suspected cases, bringing to 50 the total number of beds at Mubende.
“If we take good care of the patients even before they are confirmed cases, we give them higher chances to recover,” Dr Apiyo says.
WHO also supports local health authorities in deploying health workers and managing a fleet of 11 ambulances to transfer patients from their communities to the hospital.
Seventeen health workers are currently working at the Ebola treatment centre at Mubende, including two doctors, two clinical officers and 13 nurses.
“We plan to bring in six additional health workers and to train health workers from the Uganda People’s Defence Force who could be deployed to other regions in case the outbreak spreads further,” adds Dr Kisimu.
“One of my patients who was very sick yesterday told me today that she feels better,” says Dr Apiyo as she finally relaxes after her morning shift at Mubende, her face still bearing marks from her goggles. “I feel good when patients are doing better.”
Communication Officer
Regional Office for Africa
Email: defaitv [at] who.int (defaitv[at]who[dot]int)
Media Relations Officer
WHO Regional Office for Africa
Email: dalalm [at] who.int (dalalm[at]who[dot]int)
Tel: +254 703 245 761 (WhatsApp)