The Reproductive Health Programme works for:
- Control of Sexually Transmitted and Reproductive Tract Infections, and HIV/AIDS
- Gender Mainstreaming in Sexual and Reproductive Health
- Prevention of Cervical Cancer
- Prevention of Unsafe Abortion
- Repositioning Family Planning
Sexually transmitted infections (STIs) are transmissible mostly by sexual contact and include vaginal, oral, and anal sex. Transmission is also possible through blood products and tissue transfer. Some STIs like HIV and syphilis can be transmitted from mother to child during pregnancy and childbirth. STIs can lead to severe consequences such as fetal and neonatal death, cervical cancer, increased HIV risk, and infertility. Several other infections result from risky sexual behavior. HPV, which is responsible for almost all cervical cancer, is sexually transmitted.
Cervical cancer is the leading cause of cancer deaths in the Region. Other sexually transmitted infections such as syphilis, gonorrhea, and chlamydia, are entirely attributable to unsafe sex and still occur in several African countries.
Many STIs have the effective treatment and can be cured. The incurable STIs are caused by Human Immunodeficiency Virus (HIV), Human Papilloma virus (HPV), Herpes simplex virus (HSV), and Hepatitis B virus. Prevention of STIs is through comprehensive sexuality education, behavioral change, delayed sexual debut, promotion of safer sex, interventions targeting key populations such as sex workers, STI, and HIV pre- and post-test counseling.
The African region has the highest HIV burden globally, with 25.7 million people living with HIV and 1.1 million new infections in 2018. Adolescent girls have an increased risk because they are often married to older partners. The latter are more likely to have been exposed to HIV. About 31% of females between the ages of 20 and 24 in the African region were married before age 18.
It is also one of the leading causes of death in the region. Efforts towards the prevention and control of disease spread include access to HIV testing and counseling, promotion of female and male condom use, use of antiretroviral medicine (ARV), and elimination of mother to child transmission of HIV (EMTCT).
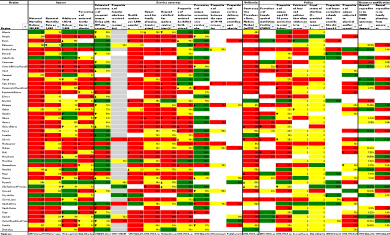
Approximately 85% of pregnant women living with HIV in the African region received ARV in 2018 to reduce the risk of prevention mother to child transmission (PMTCT) of HIV. The coverage was higher in the East and Southern African sub-regions (92%) than in the West and Central African sub-regions (59%). Besides, some countries have committed to eliminating mother to child transmission of syphilis as one of the key targets of the Global Health Sector Strategy on STIs (2016–2021), which reduces ≤50 cases of congenital syphilis per 100 000 live births in 80% of countries.
Syphilis in pregnancy can result in fetal and neonatal death. Syphilis can be detected using a rapid test kit, and there is an effective antibiotic treatment for it. In 2018, approximately 85% of pregnant women in the African region who tested positive for syphilis were treated.
Interventions
This area's main objective is to provide guidance on strategies for controlling sexually transmitted infections (STIs) and reproductive tract infections (RTIs), including strategies to prevent mother-to-child transmission of HIV and other STIs and improve processes for the integration of RH and HIV/AIDS. The following outcomes are expected:
- improved access to, and uptake of key HIV/AIDS and SRH services, a better access of people living with HIV/AIDS (PLWHA) to SRH services tailored to their needs,
- improved coverage of underserved and marginalized populations, such as injecting drug users, sex workers or men who have sex with men, with SRH services,
- greater support for dual protection against unintended pregnancy and sexually transmitted infections (STIs), including HIV, for those in need, especially young people,
- improved quality of care and enhanced programme effectiveness and efficiency.
For more information:
The SRHR and HIV Linkages Index
Sexual and Reproductive Health and Rights and HIV linkages toolkit
Gender mainstreaming is both a strategy for planning and a tool for advocacy to reduce harmful effects of the social determinants of health for men and women. However, health professionals are not adequately prepared to address women's and men's gender-specific health needs in their work. Special attention must be paid to particular groups who experience greater mortality and morbidity related to sexual and reproductive conditions than those in a better situation.
Due to a significant societal disadvantage, girls and women have limited access to health care. As an evidence of the burden of disease related to gender inequality, it is estimated that of all adults living with HIV in sub-Saharan Africa, 61% are women. Maternal mortality is also higher in developing countries than in the industrialized world. Sexual and gender-based violence affects mostly women.
Therefore, public health actors must be able to identify the factors that put women and men at risk and address these factors through effective interventions. The SRH Programme and the Gender and Women's Health Programme will support countries to seek structural changes focused on people's needs to ensure universal access to appropriate quality sexual and reproductive health care.
For more information:
Integrating female genital mutilation content into nursing and midwifery curricula: a practical guide
Person-centred communication for female genital mutilation prevention: a facilitator’s guide for training health-care providers
Country-specific estimates of unintended pregnancy and abortion incidence: a global comparative analysis of levels in 2015–2019
Learning from women’s experiences during childbirth to improve quality of care
WHO recommendations on maternal and newborn care for a positive postnatal experience
WHO antenatal care recommendations for a positive pregnancy experience
Deworming adolescent girls and women of reproductive age. Policy brief
WHO Female Genital Mutilation Cost Calculator
Global Database on the Prevalence of Violence Against Women
Cervical cancer is caused by the Human Papilloma virus (HPV). It is the second most common cancer among women living in the undeveloped regions due to late presentation and inadequate services. Human papillomavirus (HPV) is a group of viruses that are extremely common worldwide. There are more than 100 types of HPV, of which at least 14 are cancer-causing (also known as high-risk type).
Two HPV types (16 and 18) cause 70% of cervical cancers and pre-cancerous cervical lesions worldwide.
The African region has a heavy burden of Cervical Cancer due to insufficiency or lack of information and skills, lack of cervical cancer control policy, strategies and programmes, lack of collaboration and coordination of interventions, and lack of recent and comprehensive data.
In 2018, approximately 311 000 women died from cervical cancer; more than 85% of these deaths occurred in low- and middle-income countries. Cervical cancer can be cured if diagnosed at an early stage.
The risk of HPV infection leading to cervical cancer is higher among immunocompromised individuals.
HPV vaccines have been developed and approved to prevent infection from the HPV types 16 and 18, responsible for about 70% of cervical cancer cases worldwide. WHO recommends a 2-dose schedule of HPV vaccination targeting young adolescent girls aged 9-14 years old. The recommendation is 3-doses for immunocompromised and/or HIV-infected girls.
As of December 2019, only 15 countries in the African region had instituted HPV vaccination as part of the routine immunization system.
WHO recommends that women of 30 years and above undergo screening with high-performance tests for abnormal cervical cells and pre-cancerous lesions and treatment. This will aid early detection when chances for cure are higher. The age requirement does not apply to HIV positive women who are encouraged to go for screening as soon as they know their status.
Women identified with cervical disease (precancer or cancer) should receive treatment and care as part of tertiary prevention of cervical cancer.
For more information:
Human papillomavirus (HPV) nucleic acid amplification tests (NAATs) to screen for cervical pre-cancer lesions and prevent cervical cancer
WHO Cervical Cancer Prevention and Control Costing tool: human papillomavirus vaccination module (C4P-HPV tool)
WHO guideline for screening and treatment of cervical pre-cancer lesions for cervical cancer prevention
Human papillomavirus (HPV) self-sampling as part of cervical cancer screening
There are 56 million induced abortions each year worldwide.
In 2017, the African region had the highest maternal mortality ratio, estimated at 525 maternal deaths per 100,000 live births. It is estimated that 5.2% - 17.2% of maternal deaths annually in Sub-Saharan Africa are due to abortions. Abortion-related complications are hemorrhage and sepsis.
Additional consequences of unsafe abortion include lost productivity, economic burden on public health systems, stigma, and long-term health problems, such as infertility.
Providing Safe abortion and Post Abortion Care can help to reduce maternal deaths drastically in the Region.
The laws concerning a woman's right to abortion are mostly restrictive in the African region, and this promotes unsafe abortions, which can result in high rates of maternal mortality.
Most of the abortions conducted in the African countries, where it is illegal, are unsafe.
Only four countries in the African region, Angola, Cabo Verde, Sao Tome & Principe, and South Africa permit abortion to be provided legally upon the woman's request, with no justification requirement, up to a certain gestational limit.
It is entirely prohibited in Senegal, Mauritania, Madagascar, Guinea Bissau, Gabon, and Congo. In the remaining 40 countries in the region, abortion is restricted with legal permission only under certain circumstances.
A significant challenge to understanding the severity and extent of unsafe in the African region is the absence of reliable data due to the stigma and fear attached to abortion in countries, especially when it is unlawful.
Post-abortion care is the management of complications resulting from incomplete abortions or miscarriages. Health facilities (public or private) that provide primary health care services and higher levels are expected to have post-abortion care capacity.
A study, which looked at the capacity of national health systems to provide post-abortion care in 7 African countries, revealed that less than 10% of primary-level facilities could provide basic post-abortion care in 5 (71%) of those countries. In addition, less than 50% of referral facilities could provide comprehensive post-abortion care.
For more information:
WHO African Region's Countries Abortion Health Profiles
Global Abortion Policies Database
WHO Abortion care guideline
Family planning enhances efforts to improve family health. However, traditional beliefs, religious barriers, and lack of male involvement have weakened family planning interventions. Research has confirmed a high "unmet need" for family planning in sub-Saharan Africa in terms of the number or percentage of married women who say they prefer to avoid a pregnancy but are not using any contraception method.
Family planning services include counseling and provision of contraceptive methods. Modern contraception methods include oral contraceptives, implants, injectable contraceptives, intrauterine devices (IUDs), condoms (male and female), emergency contraceptive pills, lactational amenorrhea method, basal body temperature method, among others.
The proportion of the need for family planning satisfied by modern methods, Sustainable Development Goals (SDG) indicator 3.7.1, was 75.7% globally in 2019. Yet, less than half of the need for family planning was met in Middle and Western Africa.
Approximately 17% of all women in Sub-Saharan Africa and 23% of married or in-union women have an unmet need for family planning. These women would like to stop or delay childbearing but are not using any form of contraception and are thus more likely to have unplanned pregnancies or closely spaced childbirth.
Only about 28% of married or in-union women (15 – 19yrs) in the region are using modern family planning methods, and 52% have their demand for family planning satisfied by current methods.
SRH Programme is supporting countries to: (i) raise awareness at policy and political level on the benefit of family planning, (ii) develop or review family planning policies, (iii) improve the quality of family planning and other reproductive health services, and (iv) foster integration of family planning into reproductive health.
For more information:
Family Planning in the African Region
Family Planning: A Global Handbook for Providers. 2018 World Health Organization and Johns Hopkins Bloomberg School of Public Health